Understanding PCOS
Aug 20 2020, Written by Madi Hanaka, graphics by Sissi Chen, in collaboration with Dr. Laura Pipher, a naturopathic doctor focused on women’s health, and Sarah, Cheyenne, and Karishma, who have personally experienced PCOS.
This is an excerpt from a poem published in the Women’s Reproductive Health Journal by Kelly Chen. She titled it: “PCOS”. Many of us have heard this acronym thrown around from time to time, but how many of us really know what it is? What causes it? What does it mean to deal with it on a daily basis? This week, the Marlow team set out on a mission to learn more about PCOS and through our platform, we want to shed some light on how this syndrome affects those living with it.
This week’s blog post is in collaboration with Dr. Laura Pipher. Laura is a Naturopathic doctor that focuses on women’s health, specifically, period management, fertility optimization and postpartum treatments.
In preparation for this week’s blog, the Marlow team had the opportunity to chat with a few women who have first-hand experience with PCOS. To highlight a more personal perspective, Sarah, Cheyenne, and Karishma have courageously shared stories with us about their journeys through diagnosis and treatment.
What is PCOS?
“PCOS affects many as 1.4 million Canadian women. Although it is one of the most common endocrine disorders, it’s diagnosis & treatment remains unclear. This is a BIG deal! PCOS is clearly a problem affecting a huge number of women (that we know of) and their quality of life is being equally as impacted!” - Dr. Laura Pipher
Polycystic Ovarian Syndrome – while very rarely spoken of – is one of the most common endocrine disorders. PCOS affects roughly 10 million individuals worldwide, and can cause a great deal of physical and emotional pain. Before we dive into the specifics of this health condition, let’s first explore what exactly PCOS is.
From the name itself, “Polycystic Ovarian Syndrome” you could assume that one of the main characteristics of this condition is that it causes cysts to develop on one’s ovaries, and you would be (somewhat) correct. Individuals with PCOS can develop ovarian cysts, although this isn’t the case for everyone. PCOS is known to be a hormonal condition, and involves 2 major hormone groups: androgens and insulin.
-
Androgens are often referred to as “male hormones”, and those with PCOS produce a higher number of these hormones than the average female. This hyper-production of androgens leads to a number of different symptoms.
-
44%-70% of individuals with PCOS also have insulin resistance, meaning the body has difficulty absorbing glucose. Increased blood glucose levels cause the body to overproduce insulin, and spikes in insulin lead to the production of an even higher number of androgens.
What are the symptoms of PCOS?
There are many known symptoms of PCOS, many of which usually begin to appear shortly after puberty. Of course, everyone with PCOS has their own unique experience, however, one major sign that someone may have this condition is if they have an irregular menstrual cycle and/or often miss periods. Other symptoms include:
-
Ovarian cysts
-
Infertility/Difficulty getting pregnant
-
Unwanted hair growth (for example, facial hair)
-
Weight gain
-
Hair loss
-
Acne
-
Fatigue
-
Depression/Anxiety
21-year-old Sarah expressed that she was diagnosed when she was in high school, but only after “complaining enough to doctors”. It was at that point that they took notice to cysts on her ovaries during an MRI scan of her abdomen.
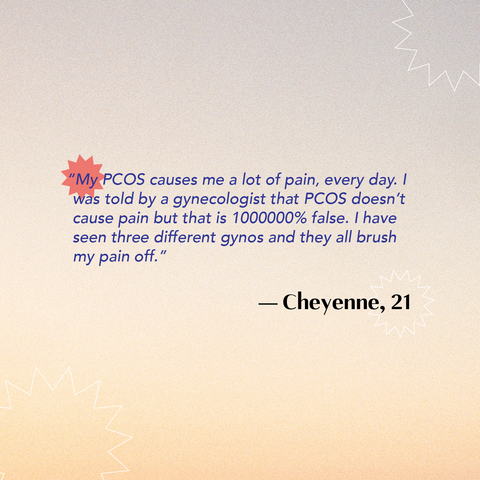
Cheyenne described a similar scenario, highlighting that the journey to her diagnosis was a somewhat lengthy process.

Karishma didn’t even go to the doctor right away, but after having a period that seemed like it was never-ending, she thought there may have been a problem.

How Does Having PCOS Affect One’s Life?
Seeing as one of the common symptoms of Polycystic Ovarian Syndrome is infertility, one of the obvious ways this condition can impact one’s life is that it may prevent certain individuals from conceiving naturally, or at all.
During our conversations with Sarah, Cheyenne and Karishma, one similarity that couldn’t go unnoticed was that all three women expressed having concerns about infertility. Despite not being ready for children at this point in their lives, they all explained that it’s difficult not to worry about not being able to conceive in the future.
Sarah for example stated:

Cheyenne described a similar feeling, explaining that although she has many fears about her PCOS, not being able to get pregnant is what scares her most.
Karishma touched on infertility as well, describing that upon her diagnosis, her doctor stressed that she would be likely to experience difficulties with fertility – especially if her PCOS were to be left untreated.
Aside from issues related to pregnancy, all three of these women also emphasized that living in pain has become part of their daily routine. Although pelvic pain is not known to be directly caused by PCOS, Sarah, Cheyenne and Karishma all reported that this is a reality they have had trouble navigating and dealing with.

For Cheyenne, being in constant pain is half the battle. She described that it has become extremely frustrating when she has been routinely dismissed by doctors.
There are unfortunately also other risks associated with PCOS beyond general pain and infertility. According to Dr. Laura Pipher, those diagnosed with PCOS are also at a higher risk of:
-
Cardiovascular Disease:
The production of excess androgens can lead to an increased risk of high blood pressure and high cholesterol levels.
-
Diabetes:
60-80% of those with PCOS have insulin resistance (lack of blood sugar control), which can lead to a diagnosis of diabetes and a whole host of associated negative health outcomes.
-
Endometrial Cancer:
Irregular periods can cause what’s called “unopposed estrogen”. As a result, the uterine lining thickens too much, increasing the risk for endometrial cancer.
-
Anxiety, Depression and Poor Self Perception:
Many of those with PCOS suffer from anxiety and depression, which negatively contributes to overall well being.
Is There a Cure for PCOS?
Unfortunately, there is no cure for PCOS; however, there are ways to treat this condition to decrease symptoms. Depending on the individual, doctors can suggest a number of different medications, for example, hormonal birth control, and/or anti-androgen and insulin medications.
Karishma and Cheyenne were initially treated with birth control after their diagnoses, although they both expressed that this seemed to only do more harm than good.

While medicinal treatment is often suggested, typically those with PCOS are also encouraged to continue managing their symptoms on their own through nutrition and exercise. Maintaining a healthy diet as well as regular physical activity is known to help reduce PCOS-related symptoms.
For Karishma, this method actually brought some success. Feeling defeated after attempting to resolve some of her symptoms with birth control, she explained that she began experimenting with managing her PCOS naturally:

She highlighted that while this method may not work for everyone, she has found it rewarding to gain some control of her own symptoms. She also emphasized how beneficial it can be to share your story with others and learn from their experiences. After posting a video about her journey with PCOS to Youtube, she was able to connect with other like minded individuals, and learn more about her own body in the process.

While of course it is important to seek out professional medical advice to prioritize your menstrual health, it is also important not to underestimate the benefits of having a community surrounding you that both relates to and supports your lived experiences.
Having open conversations with others about a health condition that is already thought to be taboo can be daunting. However, exchanging information with those who may have similar experiences, stories, and concerns can be empowering. It is important to remember that you are not alone, and that sharing your story will only encourage more dialogue around stigmatized topics like PCOS.
A special thank you to Dr. Laura Pipher for her willingness to participate in this week’s post, as well as Sarah, Cheyenne and Karishma for being so open and vulnerable. If you would like to hear more about PCOS, Additional resources from Dr. Pipher will be linked below, as well as Karishma’s Youtube video.
Video:


